COVID-19 versus the cold: what’s the difference?
Testing is the principal method of differentiating between COVID and the common cold, considering similarity in symptoms. Regardless, subtle differences in symptoms remain and understanding them can be useful.
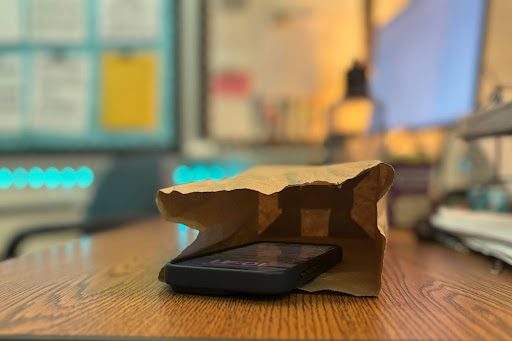
Throughout September, RM saw large numbers of student absences due to illness. While these absences could have easily been attributed to COVID-19 a year ago, now that reduced masking enables the spread of all pathogens, it is difficult to pinpoint whether COVID is still the preponderant sickness.
Many students have reported catching colds, strep throat or stomach bugs, which indicates an increase in non-COVID infections compared to last year. Indeed, as of Oct. 9, only 91 COVID cases have been self-reported at RM since Aug. 22, averaging around 15 cases per week across the entire school. This means many who were out sick did not have COVID.
The symptoms associated with COVID and the common cold are so similar that testing is the only legitimate way to distinguish the two. Even so, given the high false negative rate of rapid COVID tests—especially when symptoms are mild—checking for subtle differences in symptoms may still be informative.
According to the National Institutes of Health, while headaches, fatigue and weakness, general body aches and pains, and loss of smell are all possible symptoms of a cold, they are more common in COVID infections and should be noted during diagnosis. On the other hand, a sore throat and runny nose are equally indicative of COVID and a cold, and a fever is a typical symptom of both COVID and influenza.
As new mutations produce progressively milder variants, COVID is bearing a greater and greater resemblance to the common cold—and people are beginning to treat it that way. “I didn’t test it,” junior Zach Zhou said of his recent headache and sore throat. “I already had COVID over the summer.”
The general acceptance of COVID as endemic is reflected in the dismissive attitudes toward the virus. “Honestly, I’m kind of over it,” RM’s nurse Gene Gambo said. “You’re going to get it.”
In addition, a New York Times poll revealed that Americans are now significantly less up-to-date on COVID news than they were a year ago: although the Food and Drug Administration has already approved Pfizer’s recent Omicron-specific booster for children under 12, more than 60 percent of adults surveyed were not aware they were eligible for it. COVID is evidently no longer at the forefront of national attention.
However, the normalization of COVID does not mean that individuals are now less wary of hygiene. Instead, with the exception of consistent mask-wearing, the health-conscious habits learned from the past two years are now a hallmark of what is becoming the post-pandemic “normal.”
“[Before the pandemic], if I got a cold I would kind of neglect it and come to school anyway,” senior Eddie Fang said. “But now I take proper procedures, like making sure I don’t have a fever, taking cold medicine, and […] wearing a mask.”
While absences due to illness this past month have significantly exceeded those of this time last year, they are similar to those of pre-pandemic years and could suggest that people are more inclined than they were in past years to stay home from school when sick. These high rates of cold and strep throat may even be an indication that things are returning to normal.
“I’m fine with the current number of people getting sick and I’d say it’s expected,” Zhou said.
The increased health-consciousness that has accompanied the normalization of COVID and infectious illnesses suggests that, especially to the young and healthy, there is no longer any significant difference between COVID-19 and the common cold.
Your donation will support the student journalists of The Tide, Richard Montgomery High School's student newspaper. Your contribution will allow us to purchase equipment and cover our annual website hosting costs.
Crystal Li is a senior and The Tide’s Science Writer. She covers topics ranging from public health to technology. Outside of newspaper writing, Crystal...
Junior Claire Yu has spent two years as a News writer for The Tide, and is thrilled to work as one of the News editors this year. Her favorite aspect of...